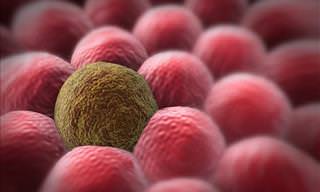
According to the results of an early-stage clinical trial published on Tuesday (26/06/2018), a genetically modified polio virus has been used to improve the longer-term survival of patients with a lethal type of brain cancer.
21% of patients treated with this virus, all with cancer that had recurred, were alive after three years, compared to just 4% of those who had undergone standard chemotherapy. The trial, that took place at the Duke Cancer Institute, involved patients suffering from glioblastoma.
This is a notoriously difficult disease to treat, but it’s one of the most common of all malignant brain tumors. It can cause headaches, blurred vision, confusion, and seizures. Even with aggressive treatment, people who are newly diagnosed rarely survive more than 20 months, while those with a recurrence usually die with a year.
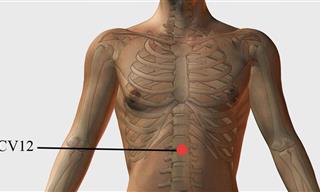
Duke researchers opened the Phase 1 trial back in 2012 to test the safety of the modified-virus treatment and to try to determine the right dose. After surgeons implanted a catheter in each patient’s brain, a small amount of a genetically modified type of the polio virus was infused directly into the tumor. The virus was designed to target the tumor cells and trigger a response by the immune system. According to Duke officials, the first participant in the trial was a nursing student who has since gotten married and become a nurse.
Tuesday’s results were welcomed by experts who were not involved in the study. However, these scientists urged caution, saying that it was too early, and the number of patients in the trial too few, to know just how effective the approach is for glioblastoma.
According to the National Cancer Institute, while researchers have long viewed such viruses as potential tools for fight cancer cells, they now suspect that the viruses might be more effective at marshaling the body’s immune system against malignancies.
The Duke researchers have said that the median survival for the 61 patients in the trial was 12.5 months, compared with 11.3 months for the “historical control group.” The latter is a group of patients, used for comparison, who were treated earlier with normal chemotherapy and met the criteria for the polio virus trial.
Debra Puffer, a 61-year-old from Rome, NY, was diagnosed with glioblastoma in 2014 and was treated using surgery, chemo, and radiation. When the cancer returned, she got the polio virus therapy at Duke and went two years without a recurrence.
When the cancer returned, she got a booster infusion of the polio virus late August. She ended up in the hospital with severe side effects. However, now, everything is looking much better.
Annick Desjardins, a Duke neurologist who is one of the lead authors of the study, said that the polio virus treatment appears similar to other immunotherapies in that the majority of treated patients don’t respond. However, those who mount “an active immune response” have the real possibility of becoming long-term survivors.
To try to increase the percentage of such responders, scientists opened a Phase 2 trial at Duke and three other medical centers to test the polio virus treatment plus a chemotherapy drug versus only the virus. Researchers are also planning trials for melanoma and breast cancer.
Deepa Subramaniam, director of the brain tumor center at Georgetown Lombardi Comprehensive Cancer Center, called the results “very interesting, enough reason to keep going.” However, she noted that it was a very early-phase trial and that the treatment needed more scrutiny.
John de Groot, a neuro-oncologist at MD Anderson Cancer Center, called the study “good science” but said the therapy’s effectiveness needed to be tested in a much larger number of patients and at many medical centers.
Both he and Subramaniam questioned the use of a historical control group, rather than an actual one. Subramaniam said that it was a “suboptimal way to compare outcomes between patients getting an experimental treatment and those receiving standard therapy.”
Desjardins said that the study authors decided a traditional randomized trial would have been unethical because those who didn’t get the treatment would have been subjected to sham procedures, such as insertion of catheters that did not deliver the virus, so that they wouldn’t know whether they were getting the experimental therapy.
Source: sciencealert
Images: depositphotos
 Go to BabaMail
Go to BabaMail