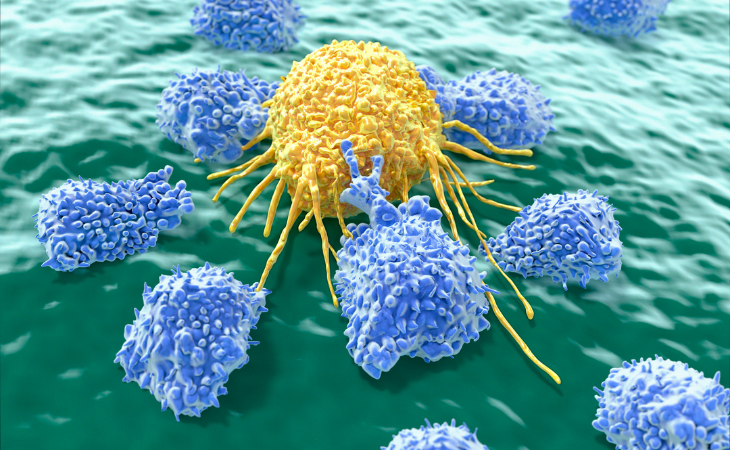
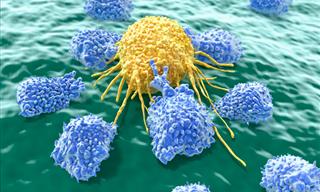
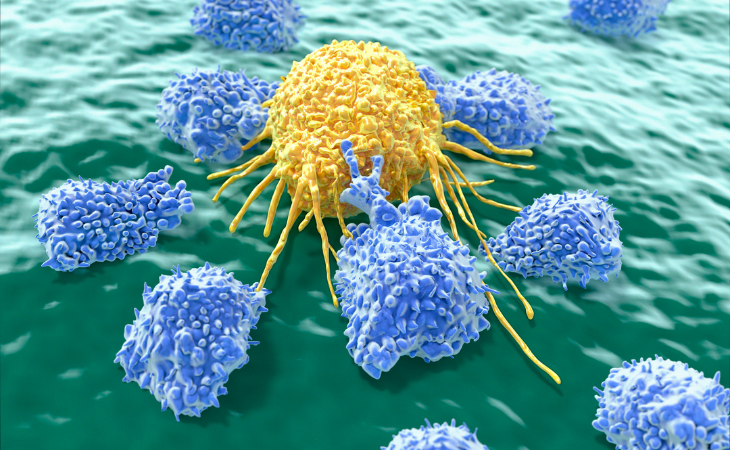
Researchers in the US have discovered a cancer cell "kill switch", activated by a specific protein segment, that can pave the way for groundbreaking treatments. This discovery, which focuses on the exterior of tumor cells, is not only significant for the development of new cancer medications, but it also indicates the potential for strengthening present therapeutic procedures for fighting cancer.
Related: Lung Cancer Pill Cuts Risk of Death by 50%
For example, it has the potential to allow chimeric antigen receptor (CAR) T-cell therapy to be used against solid tumors such as those found in the breast, lung, and prostate. The new technique involves giving cancer patients T-cells that have been precisely designed to locate and eliminate tumors.
The problem, according to Dr. Jogender Tushir-Singh, one of the researchers, is treating solid tumors since immune cells given intravenously struggle to permeate microenvironments and deliver therapeutic benefits.
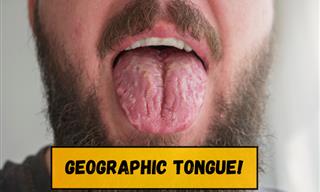
CD95 receptors, also known as Fas receptors, are found on the surface of cancer cells. When engaged, these receptors provide a signal that causes self-destruction. Despite the fact that these receptors have long been known about, attempts to activate them have been ineffective.
According to researchers at the UC Davis Comprehensive Cancer Center, a specific section on the receptor can activate the destruction process when targeted. The findings of their cell and mouse tests have been published in the journal Cell Death & Differentiation.
Dr. Tushir-Singh said: 'Now that we've identified this epitope, there could be a therapeutic path forward to target Fas in tumors.'
Related: Are You at Risk of Skin Cancer? A Guide with Pictures
Currently, conventional methods like surgery, chemotherapy, and radiotherapy remain the established protocols for treating cancer patients. However, children with leukemia and adults with lymphoma may have access to CAR T-cell therapy.

The process involves collecting and altering their own T cells, which are responsible for fighting off infections and other diseases but are unable to detect cancer cells. These customized cells are reintroduced into the bloodstream via intravenous infusion. Theoretically, these CAR T-cells are programmed to identify and combat cancer cells.
Although effective against blood cancers, there is a chance of cancer recurrence in a small percentage of patients undergoing this treatment. Additionally, patients with solid tumors currently do not have access to this treatment. Dr. Tushir-Singh suggests that, theoretically, a treatment designed to target the cancer kill 'switch' could eradicate any remaining cancer cells post-CAR T-cell therapy.
This has the potential to have a two-fold effect on cancers. Furthermore, it could support CAR T-cell treatment in solid tumors, although the mechanism is unknown. The research further indicates that individuals with a mutated epitope on their CD95 receptor fail to respond to CAR-T therapy.
Related: Scientists Believe This Purple Veg Is the Answer to Cancer
Dr. Tushir-Singh pointed out that changes in this epitope could be used to identify people who are candidates for CAR T-cell treatment. The team is presently developing a novel set of antibodies capable of attaching to and activating this specific kill switch.
However, it is unknown whether this treatment will work and, if so, which malignancies it will be able to remove. Furthermore, the lengthy process of testing means that any new therapies require years before reaching patients.
 Go to BabaMail
Go to BabaMail